Blog
Generic vs Branded Meds 2025: Same Quality, 70% Less Price?
Introduction
Standing at a pharmacy counter with a long prescription list can feel like staring at a restaurant bill that just keeps growing. For many of us managing diabetes, heart disease, asthma, or arthritis, those slips of paper do not just mean better health. They also mean a serious monthly expense.
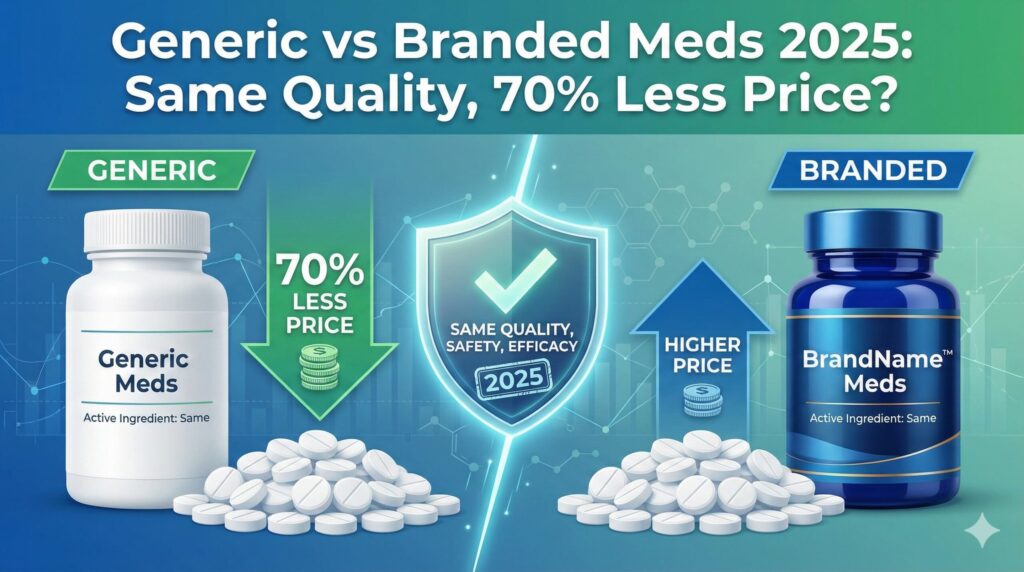
That is why a question like “Generic vs Branded Meds 2025: Same Quality, 70% Less Price?” hits so hard. It sounds almost too good to be true. If a generic pill costs a fraction of the price of a brand-name one, is it really giving the same relief, the same control of blood sugar, the same protection for the heart?
We hear this worry all the time. People tell us they are torn between what their wallet can handle and what their body needs. In this guide, we walk through how generic and branded medicines compare in 2025 using clear rules from the FDA, economic data, and real-life use.
By the end, we want readers to feel confident asking for generics when they make sense, understanding when a brand is still needed, and knowing how services like Zenerics can make long-term treatment far more affordable without giving up on quality or safety.
Key Takeaways
Before diving into details, it helps to see the big picture in a simple way. These points support the idea behind the question Generic vs Branded Meds 2025: Same Quality, 70% Less Price and guide everything that follows.
- Generic medicines use the same active ingredient, in the same strength and form, as branded drugs, and they follow the same FDA quality rules. This means they are expected to work in the body in the same way. Their lower price does not mean lower medical value.
- Savings of 70 to 90 percent are common with generics because generic companies skip the early research and huge marketing campaigns that brand makers pay for. That cost difference, not weaker medicine, explains most of the price gap people see at the counter.
- The FDA checks generics with strict bioequivalence tests that compare how the drug enters the bloodstream against the brand. Strong market competition between several generic makers then pushes prices down further, which helps patients stay on their treatment plans.
- In 2025, global supply chains, thin profit margins for generics, and possible trade rules can affect which medicines are in stock and how much they cost. Knowing how to talk with doctors, pharmacists, and trusted providers such as Zenerics helps people manage shortages and find safe, affordable options.
What Defines Generic And Brand-Name Medications

When doctors write a prescription, we often see two possible versions at the pharmacy counter. One is a well-known brand with heavy advertising. The other is a generic with a shorter, less familiar name and a much lower price. At their core, though, these two types of medicines are more alike than many people think.
A generic drug must have the same active pharmaceutical ingredient as the brand-name original. The active ingredient is the part of the medicine that actually treats the condition, such as lowering blood pressure or controlling seizures. The generic must match the brand in strength, dosage form, and route of use. So if the brand is a 20 mg tablet taken by mouth once a day, the approved generic must follow the same pattern.
The Food and Drug Administration (FDA) sets clear rules for this match. Regulators call this pharmaceutical equivalence. It means the generic and brand share the same active ingredient, same dose, same form, and same way of entering the body. The drug also has to meet the same tests for identity, strength, purity, and quality in the factory.
Where can they differ? Generics may use different inactive ingredients, also called excipients. These are fillers, binders, colorings, or coatings that help form the pill, protect it, or make it easier to swallow. That is why a generic tablet might look a different color or shape than the brand. Packaging and markings also change, because the look of the brand is protected under trademark law.
These surface differences do not change how the medicine works in the body. When the FDA approves a generic as pharmaceutically equivalent and bioequivalent, it tells patients and doctors that the generic should have the same medical effect and safety profile as the brand. In other words, the cheaper pill is designed to give the same health result.
Understanding Active Vs Inactive Ingredients
Inside every tablet or capsule there is more than just one chemical. To understand why generic pills can look different yet work the same, it helps to separate active and inactive ingredients.
The active pharmaceutical ingredient (API) is the star of the show. This is the chemical that treats the illness or controls the symptom. For example, metformin is the API that helps lower blood sugar. When we compare generic vs branded meds, this active ingredient must match exactly in type and amount.
Around that core, manufacturers add inactive ingredients. These may include:
- Fillers that give the pill bulk
- Binders that hold it together
- Coatings that help it slide down the throat
- Preservatives that keep it stable on the shelf
- Coloring agents and flavorings that change how it looks or tastes
These ingredients shape how the pill looks and handles, but they are not there to treat the disease itself.
The FDA reviews these inactive ingredients to make sure they are safe and do not interfere with how the active ingredient works or is absorbed. Different companies can choose different inactive ingredients, which is why one company’s generic tablet might be blue and another’s white. Within a single manufacturer, though, the mix stays consistent, so refills from the same source should look and feel the same.
In rare cases, a person may be sensitive or allergic to a certain dye or filler. If a rash or stomach problem starts after switching between brands or generics, it is worth sharing that pattern with a doctor or pharmacist. Often they can select a version of the same generic medicine that avoids the ingredient that is causing trouble while still keeping the cost low.
Why Generic Medications Cost 70 Percent Less The Economics Explained

Many of us hear that generics are “the same medicine” but cost 70 to 90 percent less and think there must be a catch. The real answer lies not in the pill itself but in how different companies bring those pills to market and what they spend along the way.
Brand-name drug makers start from scratch. They search through thousands of chemical ideas in the lab, test the most promising ones in cells and animals, and then run several phases of clinical trials in humans. These trials must show that the drug is safe and that it works better than a placebo or sometimes better than older treatments. This full path from early discovery to FDA approval often takes more than ten years and costs billions of dollars.
Their path usually includes:
- Discovery and preclinical testing – finding promising compounds and testing them in the lab and in animals
- Clinical trials in humans – several phases to check safety, dosing, and effectiveness
- Regulatory review – submitting a full New Drug Application and answering FDA questions
- Marketing and education – promoting the drug to doctors, hospitals, and patients
To help companies recover these costs, the law gives them patents and market exclusivity for a set period, though Prescription Drug Costs | debates continue over whether current pricing structures truly reflect these development costs or if reforms are needed. During this time, they are the only ones allowed to sell that new medicine. With no direct competition, they can charge higher prices to pay back research costs, cover manufacturing expenses, pay staff, and still make a profit. On top of that, brand makers spend large sums on advertising to doctors, hospitals, and the public.
Generic manufacturers join the story later. By the time they enter, the hard work of proving that the active ingredient is safe and useful is already done. The patent on the brand has expired, and the drug’s behavior in the body is well known. Generic companies do not repeat the long, expensive clinical trials. Instead, they file an Abbreviated New Drug Application (ANDA) with the FDA that focuses on proving they match the brand in content, quality, and how the drug moves through the body.
Skipping early research and huge marketing campaigns cuts costs sharply. In many cases, more than one generic company applies to make the same medicine. They all compete for contracts with pharmacies, insurers, and pharmacy benefit managers. To win those contracts, they keep prices as low as they can while still staying in business.
Those lower costs then flow directly to patients. Insurance plans often place generics on the lowest copay tier, and cash prices without insurance are usually much lower for generics than brands. When we ask if it is possible to have “Generic vs Branded Meds 2025: Same Quality, 70% Less Price”, the economic story explains how that big discount is possible.
“Drugs don’t work in patients who don’t take them.”
— C. Everett Koop, former U.S. Surgeon General
Lower prices for generics are one of the main reasons many people are able to stay on their medicine consistently.
The Role Of Market Competition In Driving Prices Down
Economics does not stop with the first generic maker that enters the scene. What really pushes prices down toward that 70 to 90 percent range is competition between several generic manufacturers.
When only one generic version is available, its price may sit just 20 to 30 percent below the brand. There is some savings, but not yet the deep discount most people hope for. As a second and third generic enter the market, each company fights for space on pharmacy shelves and for placement on insurance plans. The fastest way to do that is usually to offer a lower price.
This pattern shows up clearly in FDA data, and organizations tracking pharmaceutical markets confirm that Addressing Generic Drug Market challenges requires understanding how competition and supply chain factors interact to affect both pricing and availability. As the number of approved generics for a single drug rises, the average price drops in steps. By the time four or more competitors are selling the same medicine, discounts of 70 to 90 percent off the original brand price are common. The drug that once strained a family budget becomes much easier to manage month after month.
Behind the scenes, pharmacy benefit managers and large pharmacy chains often run bidding processes where generic makers offer their best prices. Brands sometimes respond by offering rebates or discounts of their own, but in many cases they cannot match the lean cost structure of generics. The FDA reported that the 773 generic applications fully approved in 2023 alone were linked with about 18.6 billion dollars in savings in their first year on the market. That is the power of competition at work for patients.
The FDA’s Rigorous Approval Process For Quality And Efficacy

One of the strongest fears we hear is simple. If a generic pill costs a fraction of the brand, is someone cutting corners on safety or quality? The FDA’s answer is clear. Generic drugs must meet the same standards as brand-name drugs in all the ways that matter for health.
When a generic company wants approval, it files an Abbreviated New Drug Application (ANDA). This application may be shorter than the original brand’s file, but it does not skip safety rules. Instead of repeating huge clinical trials, the company must prove that its product is pharmaceutically equivalent and bioequivalent to the brand.
Pharmaceutical equivalence means the generic has the same active ingredient, in the same strength, dosage form, and route of administration. A 10 mg oral tablet for blood pressure, for example, must match those same features in the brand. The FDA also checks that the generic meets clear standards for identity, strength, purity, and quality. Manufacturing plants must follow Good Manufacturing Practice (GMP) rules, just like brand factories.
The heart of the scientific review is bioequivalence testing. In these studies, healthy volunteers take the brand pill and the generic pill at different times. Researchers measure how much of the drug appears in the blood and how quickly. Then they compare the two sets of numbers using statistical rules.
For a generic to pass, the amount and speed of absorption must fall within a tight range compared with the brand. The typical standard uses a confidence interval of 80 to 125 percent for key measures, which sounds wide but in practice represents small differences that do not change how the drug works for patients. Many generics fall much closer to 100 percent.
As the FDA explains, “FDA-approved generic medicines work in the same way and provide the same clinical benefit and risks as their brand-name counterparts.”
The FDA also keeps watching after approval. Inspections, quality reports, and complaint reviews help catch any issues with manufacturing or performance. If problems appear, the agency can require corrections or even remove a product from the market. This ongoing oversight adds another layer of safety, so when we choose a generic, we are not taking a blind risk. We are using a medicine that has passed through a detailed and continuing review.
What Bioequivalence Testing Really Means For Patients
Bioequivalence can sound like a dry lab term, but it describes something very practical. It answers the question that matters most to patients: will this cheaper generic pill act the same way in my body as the brand-name pill I know?
In a typical bioequivalence study, a group of healthy volunteers takes the brand pill on one day and the generic pill on another day. Blood samples are drawn over several hours after each dose. Researchers then chart how fast the drug level rises, how high it goes, and how long it stays in the system. These curves for the brand and generic are compared.
If the generic’s curve fits closely inside the allowed range around the brand’s curve, the FDA considers the two products therapeutically equivalent. That term means they are expected to have the same clinical effect and safety profile when used in the same patients under the same conditions.
The small differences seen in these studies are usually far smaller than normal day-to-day changes in how a person’s body absorbs medicine. Eating a big meal, missing a dose, or taking a pill at a different time can cause more change than the difference between a brand and a generic that passed bioequivalence testing. Years of real-life use in clinics and pharmacies, covering billions of generic prescriptions, back up this science. For the vast majority of people, generics control blood pressure, cholesterol, blood sugar, and many other conditions just as well as branded drugs.
When Brand-Name Drugs Remain The Only Option
While generics work well for many conditions, there are times when brand-name medicines are still the only realistic choice. Knowing these cases helps set fair expectations and keeps the generic vs branded meds debate honest.
The key reason is patent protection. When a company invents a new drug, it receives patents and periods of exclusivity that can stretch ten to twenty years. During that time, no generic maker is allowed to copy the active ingredient. For newer treatments, especially for cancer, autoimmune diseases, or rare disorders, the brand may be the only version available.
This has a clear impact on spending. In the United States, brand-name drugs make up only about 15 percent of prescriptions but account for close to 90 percent of total drug costs. That heavy spending reflects the high prices often seen while patents are in force and competition is limited.
Once a patent nears its end, generic companies may prepare to enter the market. It can still take six to eighteen months before the first generic reaches pharmacies because the FDA must review and approve each ANDA. In some cases, the very first generic sets a price that is still close to the brand, so insurance plans may keep favoring the brand for a short time if it has better rebates.
Insurance formularies add another layer. Some plans place certain brands on preferred tiers or require special approval, called prior authorization, before covering them. When a brand is medically needed because no generic exists or because a patient failed on other options, doctors can provide that support.
For patients and caregivers, the best approach is open talk with the health care team. If a brand drug is straining the budget, it is fair to ask the prescriber if any lower cost options are appropriate, now or in the future when a generic becomes available. That way, the plan for care can balance both medical needs and family finances.
Navigating The 2025 Pharmaceutical Supply Chain Picture
In 2025, the question of Generic vs Branded Meds 2025: Same Quality, 70% Less Price is tied not only to science and patents but also to where and how medicines are made across the globe. The supply chain for drugs has spread across several countries, and that brings both savings and new risks.
Many high profit brand-name medicines are manufactured in European countries such as Ireland, Switzerland, and Germany, where companies benefit from business friendly tax rules and strong manufacturing bases, though the Generics-Market-Review-2025.pdf shows that European generic manufacturers face their own unique pressures in maintaining affordability while meeting quality standards. For generic drugs, production often shifts to places with lower labor and production costs, especially India and China. These centers supply a large share of the generic tablets and capsules sold in the United States.
U.S. pharmaceutical imports passed 215 billion dollars in value in 2024, which is more than double the level from a decade earlier. This heavy reliance on imports means that trade rules, shipping problems, or political tensions can all affect what shows up on pharmacy shelves. For generics, the picture is even more sensitive because manufacturers often work with very narrow profit margins.
If new tariffs or other trade measures raise the cost of importing medicines, brand-name makers with higher profits might be able to absorb some of the extra cost or shift production slowly. Generic makers, on the other hand, might struggle. Some could be forced to cut production, delay investments in quality systems, or in extreme cases exit the market for a particular drug.
Public health experts worry that this pressure could add to drug shortages or tempt weaker players to use poorer ingredients or skip needed checks. That is why choosing reliable suppliers matters. At Zenerics, for example, we focus on genuine generic medicines, double check products before dispatch, and still aim to keep prices 50 to 70 percent below branded options for patients across India. That kind of focus on both cost and careful sourcing is what patients everywhere need as supply chains grow more global and more complex.
Understanding And Addressing Generic Drug Shortages
Drug shortages are no longer rare events. They have become a regular headline and a real problem for patients. In the first three months of 2024, there were 323 drugs listed in shortage in the United States, and around 70 percent of those were generics.
Several forces sit behind these gaps:
- Intense price competition can push generic prices so low that it barely makes sense for companies to keep producing certain older drugs.
- Sterile injectables used in hospitals and critical chemotherapy agents are harder and more expensive to make, so fewer firms stay in that business.
- If one of the few remaining makers has a factory problem, fails an inspection, or decides to stop making that drug, there may not be another company ready to step in quickly.
For people who depend on these medicines, the effects are very personal. Doctors may be forced to switch patients from a first choice generic drug to a second choice brand-name option that costs more and may carry different side effects. Some patients feel tempted to stretch their remaining pills by skipping doses, which can be dangerous.
There are practical steps that can help:
- Ask the pharmacy to fill refills a bit earlier, especially for vital chronic medicines, so there is a small buffer at home.
- If a pharmacist warns about a shortage, contact the prescriber quickly to discuss safe alternatives rather than wait until the last pill.
- Check the FDA Drug Shortages Database, which lists current shortages and sometimes suggests options.
Most important, people should not ration or stop medicine on their own because of cost or stock problems. Health care teams can often adjust doses, change to another generic, move to a different brand, or help connect patients with lower cost supplies through services like Zenerics or hospital programs.
How To Access And Maximize Savings With Generic Medications
Knowing that generics and brands offer the same medical effect is only half the story. The other half is learning how to actually get those savings at the pharmacy counter. With a few clear steps, we can turn that 70 percent price promise into real money saved each month.
A simple approach is:
- Start with the prescription. When a doctor writes for a medicine, ask if there is a generic alternative and whether it is right for the condition. Many prescribers already choose generics by default, but not all electronic systems highlight them clearly, so a gentle reminder can help.
- Watch for “Dispense as Written.” If the doctor writes “Dispense as Written” or “Brand Medically Necessary,” the pharmacist may be blocked from switching to a generic without a new order. If cost is a concern, ask whether that note is essential.
- Know your state’s substitution rules.
- In some states, pharmacists must give a generic when one exists, unless the prescriber has clearly said not to.
- In other states, substitution is allowed but not mandatory, and the pharmacist might ask for agreement before changing from brand to generic.
- Compare pharmacy prices. Insurance plans usually prefer generics and place them on lower copay tiers. It still pays to compare prices across different pharmacies, including big chains, local stores, and mail order. Cash prices for generics can vary widely, and sometimes the cash price with a discount program is even lower than the insurance copay.
- Use trusted online options. Online pharmacies are another growing route. When using them, it is vital to check that the pharmacy is licensed in the United States and uses FDA approved products. For readers in India, platforms like Zenerics add another layer of support. Zenerics offers genuine generics, pan India home delivery, cashback on prepaid orders, and free shipping above certain amounts, which can make long term treatment for chronic conditions far more affordable for families managing tight budgets.
- Look for assistance programs. Manufacturer assistance programs, community health centers, and pharmacy discount cards can also lower costs, especially during times when a generic is not yet available.
By combining these tools, many patients cut their monthly medicine expenses sharply without giving up any clinical benefit, though research on Knowledge and Perception of generic medications shows that patient education remains crucial for building confidence in these cost-saving alternatives.
Working With Your Healthcare Team For Generic Options

Talking with health care professionals about money can feel awkward, but it should not, especially since Educating Patients about Generic medications effectively requires open dialogue between healthcare providers and patients about both therapeutic equivalence and financial considerations. Doctors, nurses, and pharmacists know that high costs are one of the main reasons people skip doses or stop medicine. When we bring up generics openly, we turn them into partners in finding better options.
At a new visit, we can ask simple questions such as “Is there a generic for this medicine?” or “Can we start with a generic that has a good safety record?” These questions show that cost matters and invite the prescriber to look at drug lists and formularies with us in mind. For long term medicines, it is helpful to mention any past trouble paying for refills so that cheaper choices are considered early.
When a pharmacy changes our medicine from a brand to a generic, the pill may look different even though the dose is the same. Pharmacists can explain that change and reassure us that the effect should be the same. If we notice new side effects or feel that the medicine is not working as well after a switch, it is better to call the doctor or pharmacist than to quit on our own. Sometimes the issue is simple, such as slightly different inactive ingredients from a new generic supplier.
Pharmacists are often the most reachable medicine experts in our lives. Keeping an updated list of all drugs, including brands and generics, and sharing it with both the doctor and the pharmacy helps them spot overlaps and avoid confusion. Over time, building a steady relationship with a trusted pharmacy and, where available, a reliable online provider like Zenerics makes it easier to manage changes and keep costs under control.
Conclusion
The debate wrapped in the phrase Generic vs Branded Meds 2025: Same Quality, 70% Less Price? is not just a theory problem. It is a daily decision for families trying to balance health and household budgets. The evidence from the FDA, clinical studies, and real-life experience all point in the same direction. For most conditions, generic medicines deliver the same therapeutic benefit as brand-name drugs while costing far less.
Careful FDA review, strict manufacturing rules, and detailed bioequivalence testing support the safety and performance of generics. Economics, not weaker pills, explain their lower price, and competition between multiple generic makers pushes those savings even further. At the same time, it is fair to recognize that some newer brand drugs still have no generic match and that global supply issues can cause shortages.
By asking about generics, comparing pharmacy options, and choosing trustworthy providers such as Zenerics, patients can cut costs without giving up on quality. Open talk with doctors and pharmacists about both health goals and money concerns is the key to staying on treatment. When used wisely, generics turn long term care from a constant source of stress into something a family can sustain.
FAQs
Question 1 Are Generic Drugs As Safe And Effective As Brand-Name Drugs
Yes, generic drugs are required to be just as safe and effective as brand-name medicines. The FDA checks that they have the same active ingredient, strength, dosage form, and route of use as the brand. Bioequivalence studies confirm that they enter the bloodstream in a similar way. Manufacturers must follow the same Good Manufacturing Practice rules, and billions of generic prescriptions each year show that they perform well in daily care.
Question 2 Why Do Generic Drugs Look Different From The Brand-Name Versions
Generics often look different because trademark law protects the color, shape, and markings of brand-name pills. Generic makers also choose their own inactive ingredients, such as fillers, coatings, and dyes, which can change the appearance. These changes affect how the pill looks or tastes, not how it works in the body. Within a single generic manufacturer, the appearance usually stays consistent from one refill to the next.
Question 3 Can I Switch Between Different Generic Manufacturers Of The Same Drug
In most cases, switching between generics from different manufacturers is safe. All FDA approved generics for the same drug must meet the same bioequivalence standards compared with the brand. That means they are expected to have the same medical effect and safety. If someone notices a change in how they feel after a switch, they should tell their doctor or pharmacist. Pharmacies often choose suppliers based on price and availability, but they can sometimes honor requests for a specific manufacturer.
Question 4 What Should I Do If My Insurance Does Not Cover A Generic Medication
First, it helps to ask the insurer or pharmacist to explain how the plan’s drug list is set up and why that generic is not covered. With support from the prescriber, it may be possible to request an exception so that the plan adds the medicine or lowers the copay. If that fails, patients can compare cash prices at different pharmacies, look for community programs, or ask about lower cost alternatives in the same drug class. Sometimes paying cash for a generic at a discount pharmacy is still cheaper than paying a high copay for a brand.
Question 5 How Can I Verify That My Generic Medication Is FDA Approved
People can check the FDA’s online Orange Book, which lists approved drugs and shows which generics are considered therapeutically equivalent to brands. The medicine label and patient information leaflets also carry the manufacturer’s name and approval details. Buying from a licensed pharmacy in the United States, whether in person or online, provides another level of safety. Signs of trouble include websites that offer prescription drugs without a valid prescription or prices that seem far below normal market levels.
Question 6 Will My Doctor Automatically Prescribe Generics Or Do I Need To Ask
Many doctors do choose generics first, especially for common chronic conditions, because they know generics work well and cost less. Still, it is wise to ask directly if a generic is available whenever a new drug is prescribed. Sometimes doctors mark “Dispense as Written,” which blocks substitution, so a short talk can clarify whether that is truly needed. By working together with the prescriber and pharmacist, patients can often shift safely to generic options and reduce their medicine bills over time.